In order to understand how ARDS happens in a COVID-19 patient, we must first examine the anatomy and physiology of the lungs and the role of the immune system in fighting the virus.
Lung anatomy & Physiology
Overview of the Respiratory System
- The primary function of the respiratory system is to take in oxygen and eliminate carbon dioxide. It maintains systemic arterial blood gas levels within normal range, by ensuring the following balance:
- The rates of O2 uptake and CO2 excretion at the lungs must match the respective rates of O2 use and CO2 production by cellular respiration.
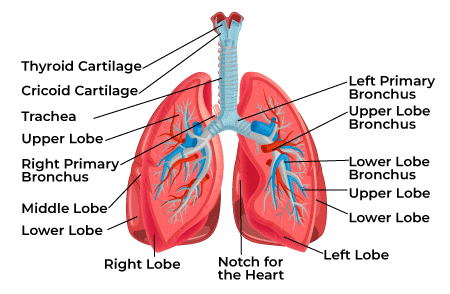
- The main components of the respiratory system are the lungs, the chest wall, and the pulmonary blood vessels.
- Muscles of the chest wall power the movement of air into the lungs during inspiration.
- Distribution of the pulmonary blood flow, to match ventilation, ensures the proper gas exchange.
- The levels of systemic O2 and CO2 are monitored by chemoreceptors, allowing the pulmonary system to respond to changes in cellular respiration.
Blood-Gas Interface
- The lung is specialized for gas diffusion and has an internal surface area of 50–100 m2.
- The large surface area is produced by several branching of the airways, which begins at the trachea and terminates in aprox. 600 million closed air sacs called alveoli.
- Ventilation is the process whereby air enters the lungs and comes into contact with alveoli, which are the sites of gas exchange.
- Each alveolus is surrounded by a dense network of pulmonary capillaries.
- The blood gas interface is less than 1-?m thick and consists of the following four elements in series
- Thin layer of surface liquid.
- Alveolar lining cells (type 1 pneumocytes), plus associated basement membrane.
- Thin layer of interstitial fluid.
- Pulmonary capillary endothelial cells, plus associated basement membrane.

- The layers of cells lining the alveoli and the surrounding capillaries are each only one cell thick and are in very close contact with each other.
- Oxygen passes through this air-blood barrier into the blood in the capillaries? Oxyhemoglobin (HbO2)
- Carbon dioxide passes from the blood into the alveoli and is then exhaled.
- Oxygenated blood travels from the lungs through the pulmonary veins and into the left side of the heart, which pumps the blood to the rest of the body
- Oxygen-deficient, carbon dioxide-rich blood returns to the right side of the heart through two large veins, the superior vena cava and the inferior vena cava.
- Blood is pumped through the pulmonary artery to the lungs, where it picks up oxygen and releases carbon dioxide.
Pathophysiology of Acute Respiratory Distress Syndrome (ARDS)
- Acute respiratory distress syndrome (ARDS) is breathing failure that can occur in critically ill persons with underlying illnesses.
- It is not a specific disease. Instead, it is a life-threatening condition that occurs when there is severe fluid buildup in both lungs.
- The fluid buildup prevents the lungs from working properly? impairment of transfer of oxygen from air into the body and carbon dioxide out of the body into the air.
- In ARDS, the capillaries (tiny blood vessels) in the alveoli of the lungs are damaged because of an infection, injury, blood loss, or inhalation injury.
- Fluid leaks from the blood vessels into the alveoli. While some alveoli fill with fluid, others collapse? lungs can no longer fill properly ? stiffness.
- Without air entering the lungs properly? the amount of oxygen in the blood (PO2) drops? patient must be given extra oxygen and may need to be ventilated
- Breathing failure can occur very quickly after the condition begins.
- It may take only 1 or 2 days for fluid to build up.
- The process that causes ARDS may continue for weeks.
- If scarring occurs, this will make it harder for the lungs to take in oxygen and get rid of carbon dioxide.
In the past, only about 4 out of 10 people who developed ARDS survived. But today, with good care in a hospital’s intensive or critical care unit, many people (about 7 out of 10) with ARDS survive. Although many people who survive ARDS make a full recovery, some survivors have lasting damage to their lungs.
What causes ARDS?
The causes of acute respiratory distress syndrome (ARDS) are not well understood. It can occur in many situations and in persons with or without lung disease.
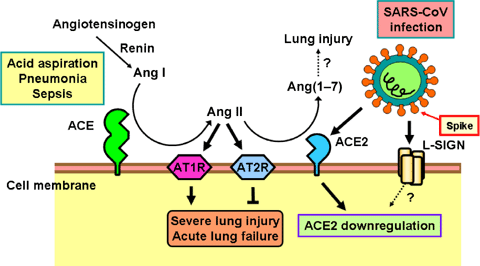
There are two ways that lung injury leading to ARDS can occur:
1- Direct lung injury
A direct injury to the lungs may result from breathing in harmful substances or an infection in the lungs. Some direct lung injuries that can lead to ARDS include:
Severe pneumonia (infection in the lungs)
Breathing in vomit/ stomach contents
Breathing in harmful fumes or smoke
A severe blow to the chest or other accident that bruises the lungs
2- Indirect lung injury
- Severe and widespread bacterial infection in the body (sepsis)
- Severe injury with shock
- Severe bleeding requiring blood transfusions
- Drug overdose
- Inflamed pancreas
Signs and symptoms of ARDS
The major signs and symptoms of acute respiratory distress syndrome (ARDS) are:
Shortness of breath
Fast, labored breathing
A bluish skin color (due to a low level of oxygen in the blood)
A lower amount of oxygen in the blood
ARDS is often associated with the failure of other organs and body systems, including the liver, kidneys, and immune system. Multiple organ failure often leads to death.
How is ARDS diagnosed?
Doctors diagnose acute respiratory distress syndrome (ARDS) when:
A person suffering from severe infection or injury develops breathing problems.
A chest X-ray shows fluid in the air sacs of both lungs.
Blood tests show a low level of oxygen in the blood.
Other conditions that could cause breathing problems have been ruled out.
ARDS can be confused with other illnesses that have similar symptoms. The most important is congestive heart failure. In congestive heart failure, fluid backs up into the lungs because the heart is weak and cannot pump well. However, there is no injury to the lungs in congestive heart failure. Since a chest X-ray is abnormal for both ARDS and congestive heart failure, it is sometimes very difficult to tell them apart.
How is ARDS treated?
Patients with acute respiratory distress syndrome (ARDS) are usually treated in the intensive or critical care unit of a hospital. The main concern in treating ARDS is getting enough oxygen into the blood until the lungs heal enough to work on their own again. The following are important ways that ARDS patients are treated.
Drugs to relieve anxiety and keep the patient calm and from “fighting” the breathing machine
Drugs to raise blood pressure or stimulate the heart
Muscle relaxers to prevent movement and reduce the body’s demand for oxygen
Other treatments
With breathing tubes in place, ARDS patients can not eat or drink as usual. They must be fed through a feeding tube placed through the nose and into the stomach. If this does not work, feeding is done through a vein. Sometimes a special bed or mattress, such as an airbed, is used to help prevent complications such as pneumonia or bedsores. If complications occur, the patient may require treatment for them.
Tidal Volume (TV)
TV: The volume of air breathed in and out at rest
- Volume: 500 ml in an average built adult male
- Behavior in restrictive lung diseases:
- The tidal volume tends to decrease
- the lungs fail to expand properly as a result of restrictive forces exerted from within the lungs (e.g. – fibrosing alveolitis) or from the thoracic wall (e.g. – severe scoliosis, ankylosing spondylitis).-
- Weakness of the respiratory muscles (e.g. – myasthenia gravis, Guillain Barre syndrome and phrenic nerve palsy) can also give rise to restricted movements of the chest wall resulting in the reduction of the tidal volume.
Inspiratory Reserve Volume (IRV) and Expiratory Reserve Volume (ERV)
- The inspiratory reserve volume (IRV): The amount of air that can be inhaled in addition to the tidal volume ie the additional amount of air, the lungs can accommodate during a deep inspiration
- Volume:aprox. 3 L
The expiratory reserve volume (ERV): The amount of volume that can be exhaled, in excess to the tidal volume
Volume: approx. 1.3 – 1.5 L.
Residual Volume (RV)
- The residual volume (RV): The volume, which cannot be expelled even after a maximally forceful expiration
- The lungs do not collapse completely following a deep, forceful expiration. A certain volume of air remains within the lungs, maintaining the alveoli expanded and the airways patent.
Four capacities have been described based on the four lung volumes:
- Inspiratory Capacity (IC) is the maximum volume of air that can be inhaled following a resting state. This can be calculated by the addition of tidal volume and the IRV.
- Vital Capacity (VC) is the maximum volume of air that can be exhaled following a deep inspiration. This is the total of IRV + TV + ERV.
- Functional Residual Capacity (FRC) is the volume of air that remains in the lungs during quite breathing. FRC = ERV + RV.
- Total Lung Capacity (TLC) is the volume the whole respiratory system can accommodate. Therefore, TLC= IRV + TV + ERV + RV.

Acute respiratory distress syndrome (ARDS) is a type of respiratory failure characterized by the rapid onset of widespread inflammation in the lungs. Symptoms include shortness of breath (dyspnea), rapid breathing (tachypnea), and bluish skin coloration (cyanosis).